A Novel Deep Learning Framework for the Detection of Tuberculosis using Chest X-ray Images
DOI:
https://doi.org/10.26438/ijcse/v12i6.1320Keywords:
Machine learning, Tuberculosis, Deep learnin, Chest X-ra, Radiological imagesAbstract
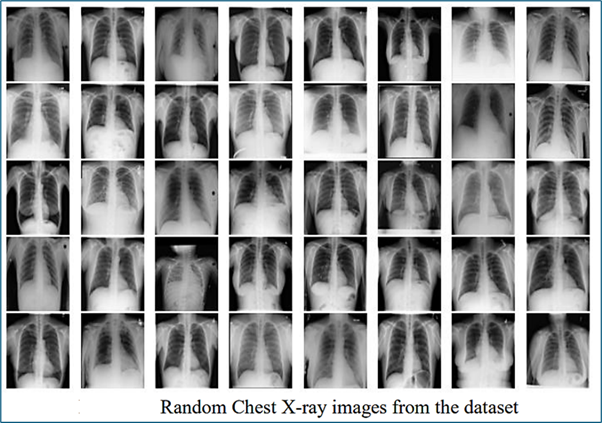
Machine learning can play an important role in changing the dynamics of the modern healthcare system. In terms of the diagnosis field, Machine learning algorithms have offered tremendous support to Radiologists, healthcare workers, and other decision-makers. Early diagnosis of TB can stop the further spread and eventually mortality rate due to TB will fall. Currently, the standard method that is used for the diagnosis of TB takes one to four weeks while the rapid test takes 24 hours, so using Radiological images has an advantage over the existing standard method. In this paper, we have proposed a Novel Framework based on the application of Deep Learning to detect Tuberculosis (TB) using Chest X-ray images. In this work, 4200 images have been used to train the deep learning model. The model has achieved an accuracy of 99.41% in classifying Normal Chest X-rays and Tuberculosis (TB) Chest X-rays.
References
[1] D. Verma, C. Bose, N. Tufchi, K. Pant, V. Tripathi, and A. Thapliyal, “An efficient framework for identification of Tuberculosis and Pneumonia in Chest X-ray images using Neural Network,” Procedia Comput. Sci., Vol.171, No.2019, pp.217–224, 2020, doi: 10.1016/j.procs.2020.04.023.
[2] G. M. M. Alshmrani, Q. Ni, R. Jiang, H. Pervaiz, and N. M. Elshennawy, “A deep learning architecture for multi-class lung diseases classification using Chest X-ray (CXR) images,” Alexandria Eng. J., 2022, doi: 10.1016/j.aej.2022.10.053.
[3] S. Shastri, S. Kumar, K. Singh, and V. Mansotra, “Designing Contactless Automated Systems Using IoT, Sensors, and Artificial Intelligence to Mitigate COVID-19,” Internet of Things, pp.257–278, Mar. 2022, doi: 10.1201/9781003219620-13.
[4] L. J. Muhammad, E. A. Algehyne, S. S. Usman, A. Ahmad, C. Chakraborty, and I. A. Mohammed, “Supervised Machine Learning Models for Prediction of COVID-19 Infection using Epidemiology Dataset,” SN Comput. Sci., Vol.2, No.1, 2021, doi: 10.1007/s42979-020-00394-7.
[5] S. Khan and T. Yairi, “A review on the application of deep learning in system health management,” Mech. Syst. Signal Process., Vol.107, pp.241–265, 2018.
[6] S. Shastri, P. Kour, S. Kumar, K. Singh, and V. Mansotra, “GBoost: A novel Grading-AdaBoost ensemble approach for automatic identification of erythemato-squamous disease,” Int. J. Inf. Technol., Vol.13, No.3, pp.959–971, 2021, doi: 10.1007/s41870-020-00589-4.
[7] L. Martinez et al., “Infant BCG vaccination and risk of pulmonary and extrapulmonary tuberculosis throughout the life course: a systematic review and individual participant data meta-analysis,” Lancet Glob. Heal., Vol.10, No.9, pp.e1307–e1316, 2022, doi: 10.1016/S2214-109X(22)00283-2.
[8] T. R. Soares et al., “Evaluation of Chest X-ray with automated interpretation algorithms for mass tuberculosis screening in prisons: A cross-sectional study,” Lancet Reg. Heal. - Am., Vol.17, p. 100388, 2023, doi: 10.1016/j.lana.2022.100388.
[9] O. Hrizi et al., “Tuberculosis Disease Diagnosis Based on an Optimized Machine Learning Model,” J. Healthc. Eng., Vol.2022, 2022, doi: 10.1155/2022/8950243.
[10] S. M. Fati, E. M. Senan, and N. ElHakim, “Deep and Hybrid Learning Technique for Early Detection of Tuberculosis Based on X-ray Images Using Feature Fusion,” Appl. Sci., Vol.12, No.14, 2022, doi: 10.3390/app12147092.
[11] R. Mehrrotraa et al., “Ensembling of Efficient Deep Convolutional Networks and Machine Learning Algorithms for Resource Effective Detection of Tuberculosis Using Thoracic (Chest) Radiography,” IEEE Access, Vol.10, no. June, pp.85442–85458, 2022, doi: 10.1109/ACCESS.2022.3194152.
[12] C. Liu et al., “TX-CNN: Detecting tuberculosis in Chest X-ray images using convolutional neural network,” Proc. - Int. Conf. Image Process. ICIP, vol. 2017-Septe, pp.2314–2318, 2018, doi: 10.1109/ICIP.2017.8296695.
[13] R. Mohan, S. Kadry, V. Rajinikanth, A. Majumdar, and O. Thinnukool, “Automatic Detection of Tuberculosis Using VGG19 with Seagull-Algorithm,” Life, Vol.12, No.11, pp.1848, 2022, doi: 10.3390/life12111848.
[14] E. Showkatian, M. Salehi, H. Ghaffari, R. Reiazi, and N. Sadighi, “Deep learning-based automatic detection of tuberculosis disease in Chest X-ray images,” Polish J. Radiol., Vol.87, No.1, pp.118–124, 2022, doi: 10.5114/pjr.2022.113435.
[15] A. S. Becker et al., “Detection of tuberculosis patterns in digital photographs of Chest X-ray images using Deep Learning: Feasibility study,” Int. J. Tuberc. Lung Dis., Vol.22, No.3, pp.328–335, 2018, doi: 10.5588/ijtld.17.0520.
[16] M. Ayaz, F. Shaukat, and G. Raja, “Ensemble learning based automatic detection of tuberculosis in Chest X-ray images using hybrid feature descriptors,” Phys. Eng. Sci. Med., Vol.44, no.1, pp.183–194, 2021, doi: 10.1007/s13246-020-00966-0.
[17] L. Wang et al., “Distinguishing nontuberculous mycobacteria from Mycobacterium tuberculosis lung disease from CT images using a deep learning framework,” Eur. J. Nucl. Med. Mol. Imaging, Vol.48, No.13, pp.4293–4306, 2021, doi: 10.1007/s00259-021-05432-x.
[18] F. Weng et al., “Differentiation of intestinal tuberculosis and Crohn’s disease through an explainable machine learning method,” Sci. Rep., Vol.12, No.1, pp.1–12, 2022, doi: 10.1038/s41598-022-05571-7.
[19] N. Sasikaladevi, “Deep learning framework for the robust prognosis of Tuberculosis from radiography images based on fused linear triangular interpolation,” 2022.
[20] L. An et al., “Article E?TBNet: Light Deep Neural Network for Automatic Detection of Tuberculosis with X?ray DR Imaging,” Sensors, Vol.22, No.3, 2022, doi: 10.3390/s22030821.
[21] R. H. Abiyev and M. K. S. Ma’aitah, “Deep Convolutional Neural Networks for Chest Diseases Detection,” J. Healthc. Eng., Vol.2018, pp.4168538, 2018, doi: 10.1155/2018/4168538.
[22] Z. Z. Qin et al., “Using artificial intelligence to read Chest radiographs for tuberculosis detection: A multi-site evaluation of the diagnostic accuracy of three deep learning systems,” Sci. Rep., Vol.9, No.1, pp.1–10, 2019, doi: 10.1038/s41598-019-51503-3.
Downloads
Published
How to Cite
Issue
Section
License

This work is licensed under a Creative Commons Attribution 4.0 International License.
Authors contributing to this journal agree to publish their articles under the Creative Commons Attribution 4.0 International License, allowing third parties to share their work (copy, distribute, transmit) and to adapt it, under the condition that the authors are given credit and that in the event of reuse or distribution, the terms of this license are made clear.




